See Part 1, Part 2, Part 3 , Part 4 and Part 5 of The Unraveling of Ryan, an anonymous testimony. Permission is required to reproduce the story. Names are changed, but details are accurate.
As a child, I was stung by bees several times. Each time my reaction got progressively worse. The last time it happened was at age 16; the doctor told me I could die if it happens again. Why is marijuana use like a fatal bee sting that makes some people swell until they implode? So many young people develop adverse effects from using today’s high-strength pot. Just because marijuana originated in nature doesn’t make it safe.
Research around the globe proves that marijuana causes panic attacks, paranoia, severe anxiety and/or depression. American hospitals often don’t consider marijuana a factor in the picture of mental health, and that’s a tragedy. There’s an urgent need for psychiatry to train more addiction specialists. If users quit after the first episode of psychosis or mental health condition, they probably can avoid a permanent psychological problem. However, these users must never go back to pot again. It’s like avoiding the bee stings if someone who’s allergic doesn’t want a fatal reaction, or like someone in Alcoholics Anonymous who can’t take one drink again.
 My nephew Jason, is one that followed this advice. In 2011, when he was 16, he experimented with marijuana and developed severe anxiety and panic attacks. Ryan was still alive at the time. My brother and his wife took him to his pediatrician, who referred him to a psychiatrist, a psychologist and a pediatric neurologist. Each doctor insisted that pot could not be the cause of Jason’s severe anxiety, panic attacks and sweats. Maybe they didn’t realize that the highly potent pot in California today has 12-15 % THC, at least 5x what it was when those doctors were in school.
My nephew Jason, is one that followed this advice. In 2011, when he was 16, he experimented with marijuana and developed severe anxiety and panic attacks. Ryan was still alive at the time. My brother and his wife took him to his pediatrician, who referred him to a psychiatrist, a psychologist and a pediatric neurologist. Each doctor insisted that pot could not be the cause of Jason’s severe anxiety, panic attacks and sweats. Maybe they didn’t realize that the highly potent pot in California today has 12-15 % THC, at least 5x what it was when those doctors were in school.
He survived because he stopped using pot, made more urgent after attending his oldest cousin Ryan’s funeral. He was never hospitalized and his brain fully recovered in nine months. Today, Jason plays Division 1 basketball in college. When I saw my brother at Thanksgiving, he thanked me for sharing the knowledge about marijuana that has kept Jason alive and thriving.
I’ve read about the COMT gene polymorphism which explains why there may be a genetic link for anyone who carries the recessive gene allele, about 25% of the world population. I contacted three researchers around the globe in hopes of getting my family’s blood analyzed. Even though the research has been published, a blood test for DNA recognition of this gene identification is at least 10 years away.
Stopping a Problem in its Tracks
A young neighbor recently confessed he was a big pot user all through high school. Suddenly, he’s been dealing with his mother’s unexpected illness and the stress of a job change. He developed anxiety out of nowhere, but felt it was related to his marijuana use. His friends keep pushing him to use pot, and to use even more than he had before. (How could someone who would goad another young person to use pot be called a “friend?”) Thankfully, this young man listened to his own body and mind.
Now I’ve heard that Amanda Bynes has gotten her life back on track. As of late December, she plans to go to college, stay sober and study psychology. Congratulations and best wishes for her continual recovery. Let’s hope this time she realizes that returning to marijuana could easily lead her to permanent psychosis.

A Story from Colorado
On a cruise to Alaska with my mother, a story emerged from a couple living in Colorado. Their 21-year-old son had developed depression, out of nowhere. The mom wasn’t concerned her son was smoking pot with his college roommates. “It’s just pot and I smoked while at UCLA in the 70s.” By the end of dinner, she wanted to heliport herself back home to save her son, because of the tragic events I had shared about my son and the high THC content of today’s cannabis.
It was when she finally said her son does too much pot with his friends that I couldn’t hold my tongue. Her boyfriend (not the boy’s father) was Dutch and had a ponytail, so I had instantly judged him to be cool with marijuana, since there have been marijuana coffeehouses for decades in Amsterdam. To my shock, he said that lawmakers in the Netherlands recently capped the strength of pot!! Then this woman blurted: “Tim’s been attending a drug education series at the local Sheriff’s Department for several weeks. He’s been telling me the same thing about pot as you did, but I’ve been blowing him off, as though it was just “‘crazy talk.’”
Afterwards I felt upset that I had violated my vow not to discuss anything about pot or my son Ryan when I boarded the ship. My mom saw the woman later and said: “You just may have saved that young man’s life.” Her boyfriend had been feeding her the same facts I had, but she continued in denial until hearing the story of my son’s pot use and my belief that it led to his tragic demise.
Wake up, America to the Looming Mental Health Crisis
After losing my own kid, I caution parents not to live in denial of marijuana, as I did. Your child will be exposed to marijuana and is likely to experiment with it. It is my mission to prevent other young people from going down the same path my son did.
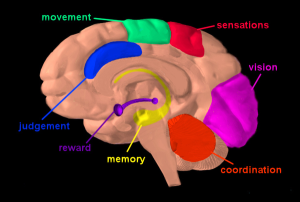
If a person who uses today’s highly potent marijuana goes into psychosis (or depression, panic attack, other psychiatric presentation), the mental health system needs to first address the drug effects and the need for addiction treatment. Next, educate the person about brain health and wait for the drug-induced mental illness to run its course.
In California, which has unregulated medical marijuana, it’s been common to rope young marijuana users with psychotic symptoms into the label of a permanent, debilitating mental illness rather than give them addiction treatment. For some, the diagnosis of bipolar disorder may be more comforting than advising them of the absolute need to give up marijuana. When it comes to strong males like my son, they also flood them with powerful, unnecessary pharmaceutical drugs.
Our children and teens need to learn the true harms about today’s pot, especially to their, young, developing brains. The marijuana financiers should stop pretending they know about medicine. Medical marijuana practitioners are doing far more harm than good, as the one who gave pot to my friend Leah’s son, Brandon.
A new Ventura County website suggests that some communities might be waking up from these delusions brought on by changing social norms, and “medical marijuana.” Just because something originates in nature doesn’t mean it’s safe. Like some people die from a bee sting, a part of mother nature, some people die from the consequences of using marijuana, or they spiral out of control.
If marijuana is legalized nationally, the need for mental health treatment will explode. Psychiatry is a tricky field with less success than other medical specialties, like heart disease or emergency medicine. The fallout will be huge. Wake up, America. We are in uncharted waters, as marijuana use is growing nationwide and your kid may be the next casualty.