By Ken Finn, MD, Springs Rehabilitation, PC, Colorado Springs

Dr. Sanjay Gupta has been supporting the use of marijuana to curb the opioid crisis. Dr. Gupta does not have specialty training in Pain Medicine, Physical Medicine and Rehabilitation, Pain Management, or Anesthesia. I have been practicing Pain Medicine in Colorado for 24 years and I have seen patients referred to me on very high dose opioids, reporting very high levels of pain, and using marijuana for pain control, making no clinical sense. In discussions with these patients, and overall, a significant percent report that their use of marijuana does not help with their presenting pain symptoms. I have had a rare patient who opt to taper their opioids and use marijuana, and all of those continue to report high levels of pain.
In my clinical practice, patients openly report sharing their medical marijuana. After their medical marijuana card expires, they grow their own marijuana. Now, with a legal layer of marijuana in Colorado, people are self diagnosing and treating their medical conditions without physician supervision.
When drug testing patients who are on chronic opioid therapy, it’s been my experience that many patients, independently, and without my knowledge, tend to also co-treat with marijuana and tend to be positive for other illicit substances, which is consistent with the literature.
The evidence for treating marijuana for pain
Pain is a broad diagnosis and different types of pain will respond to different kinds of medications. As it relates to the use of marijuana for pain, there is some evidence there are components of the plant which may help in different pain conditions.
It is important to understand the current evidence on pain involves studies totaling about 2,500 patients. Some of these studies are low in number, short in duration and not placebo-controlled. The National Academies of Science, Engineering and Medicine report misleadingly stated, “There is substantial evidence that cannabis is an effective treatment for chronic pain in adults.” Even in their own review, the NAS noted that most of the studies on pain used nabiximols (natural, purified, controlled; Sativex), which is not available in the United States, or were with synthetics (dronabinol, marinol), which would be considered “off label” use and likely not covered by insurance. Furthermore, the conditions studied were most often neuropathic pain or cancer pain. (Read Current Research on Marijuana for Pain ).
Currently there is no available accepted medical literature showing any benefit with dispensary cannabis in common pain conditions, which was noted in the Annals of Internal Medicine, August 2017.
No evidence marijuana can curb the opioid epidemic
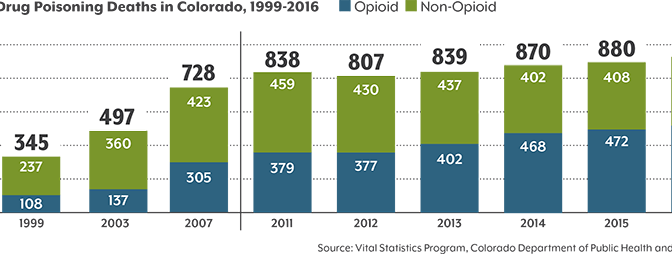
As it relates to curbing the opioid epidemic, it simply is not happening in Colorado. Last year, 2017, was a record year of opioid overdose deaths. Colorado Department of Public Health and Environment has been monitoring this data over time.
The Journal of Public Health reported that opioid overdose deaths were on the decline. However, the report did not take several things into consideration, such as: widespread use of Narcan, physicians becoming more cautious in the wake of epidemic and patients becoming more reluctant to accept opioids. This was also during a period of time where prescriptions were moving to long acting agents and abuse deterrent formulation.
Over time, opioid overdoses have continued to climb in Colorado, despite having a medical marijuana program since 2001. Of greater concern–in Colorado–the opioid epidemic has been morphing into a more widespread problem with methamphetamine and cocaine making a comeback and causing increasing deaths in Colorado (See below). I would be brave enough to state that marijuana is a companion drug rather than a substitute and is contributing to the opioid epidemic in Colorado.
Cannabis use can result in higher rates of opioid abuse
American Journal of Psychiatry released an important paper September 2017. Following 33,000 people, the study showed that cannabis use increases the risk of non-medical prescription opioid use and opioid use disorder.
Regarding the association between cannabis use and aberrant behavior during chronic opioid therapy for chronic pain, it has been shown that patients using cannabis and opioid concurrently have a higher risk of opioid misuse (Pain Medicine 2017; 0: 1–12). Additionally, people using cannabis for pain were more likely to meet criteria for substance use disorders and more likely to be noncompliant with their prescription opioids (Evidence Based Practice 2017; 20(1), e10; attached). Even patients in with chronic pain in an interdisciplinary pain rehabilitation program may be at higher risk for substance-related negative outcomes and are more likely to report a past history of illicit substance use, alcohol use, and tobacco use (J Subst Abuse Treat. 2017 Jun; 77: 95-100; attached).
Finally, a more recent article showed medical marijuana users were more likely to report prior use of prescription drugs, including pain relievers, stimulants and tranquilizers (J Addiction Medicine, 2018).
Marijuana use is NOT helping the opioid epidemic, and the science demonstrates it may be contributing the opioid epidemic. Dr. Gupta needs to be careful regarding providing misleading information to the public.
Kenneth Finn, MD Board Certified, Physical Medicine and Rehabilitation Board Certified, Pain Medicine Board Certified, Pain Management Member, American Academy of Physical Medicine and Rehabilitation Member, American Academy of Pain Medicine Member, American Board of Pain Medicine, Exam Council Member, American Board of Pain Medicine, Executive Board